Colectomy is a major surgical procedure used to treat conditions affecting the colon, such as cancer, inflammatory bowel disease, and other serious disorders. At Colorectal Practice, we offer colorectal surgery in Singapore to help patients manage colorectal cancer and related gastrointestinal conditions.
What Is Colectomy?
Why Is Colectomy Done
Colectomy is performed for several reasons, including:
- Colorectal Cancer: To remove cancerous sections of the colon
- Inflammatory Bowel Disease: To treat conditions like Crohn's disease and ulcerative colitis, when medications are ineffective
- Diverticulitis: To treat severe or recurrent inflammation of diverticula in the colon
- Bowel Obstruction: To relieve a blockage that prevents normal bowel movement
- Severe Bleeding: To control persistent or life-threatening bleeding in the colon
- Perforation: To repair a hole in the colon wall and prevent infection
What Are the Different Approaches to Performing Colectomy?
There are two methods used to perform colectomy, each with its own advantages and indications:
Open Colectomy
In an open colectomy, the surgeon makes a large incision in the abdominal wall to directly access the colon. The open approach allows the surgeon to examine the colon directly, which can be helpful in complex cases such as those involving severe inflammation or scarring.
Laparoscopic Colectomy
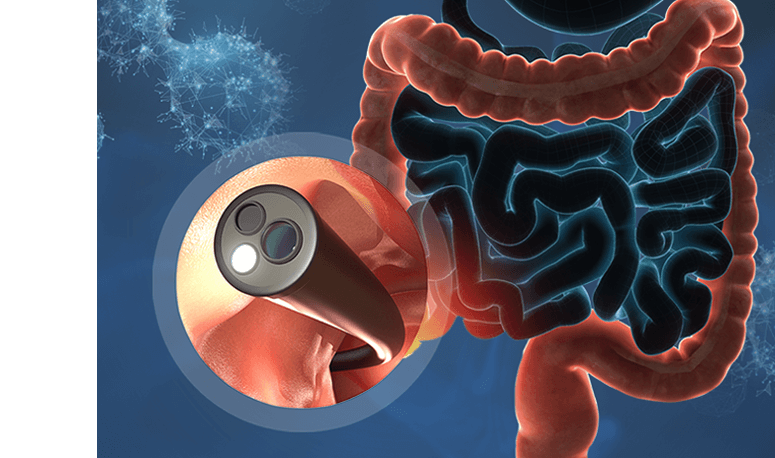
Laparoscopic colectomy uses several small incisions through which a camera (laparoscope) and specialised instruments are inserted. The magnified video feed guides precise dissection and resection, reducing tissue trauma. Compared to open surgery, laparoscopic approaches typically lead to less postoperative pain, shorter hospital stays, and faster return to normal activities.
How Do You Prepare for a Colectomy?
Preparing for a colectomy involves several steps to ensure a safe and successful surgical experience. Each of these steps plays a crucial role in reducing risks and enhancing recovery.
- Pre-Operative Counselling — Preoperative counselling is essential for setting patient expectations and providing detailed information about the surgery.
- Bowel Preparation — Patients usually need to undergo bowel preparation before surgery. This usually involves a clear liquid diet, laxatives, and sometimes antibiotics to lower infection risk. Emptying the colon helps surgeons perform the procedure more safely and effectively.
- Medications to Stop or Adjust — Certain medications need to be stopped or adjusted before surgery to minimise risks.
What To Expect During a Colectomy
Open Colectomy
Open colectomy involves making a single, long incision in the abdomen to access the colon directly. This traditional method allows surgeons to visually inspect and manually remove the affected portion of the colon. It is often used in emergencies or when more extensive access is required. Key steps include:
- Anaesthesia — Patients will be placed under general anaesthesia for their comfort.
- Incision and Exposure — A large incision is made along the midline of the abdomen to fully expose the colon.
- Removal and Reconstruction — The surgeon removes the affected segment of colon, then either reconnects the healthy ends (anastomosis) or creates a stoma, which is an opening to divert waste into a bag outside the body, if needed.
Laparoscopic Colectomy
Laparoscopic colectomy is a minimally invasive technique that uses several small incisions and a camera to perform the surgery. This approach generally results in less postoperative pain and faster recovery. Key steps include:
- Anaesthesia — General anaesthesia is administered to ensure patient comfort.
- Incision & Insufflation — A few small incisions are made in the abdomen, and carbon dioxide gas is used to inflate the abdominal cavity for better visualisation.
- Mobilisation & Resection — The surgeon uses specialised instruments to free the affected part of the colon, divide its blood supply, and remove it.
- Specimen Extraction & Anastomosis — The removed segment is placed in a bag and extracted through one of the incisions. The healthy parts of the bowel are then reconnected, either inside the abdomen or through the incision.
What To Expect After Colectomy
Recovery from colectomy varies significantly depending on whether the procedure is performed using an open or a laparoscopic colectomy. The recovery times are as follows:
- Open Colectomy — Recovery typically involves a hospital stay of 6 to 11 days. Full recovery at home can take 6 to 8 weeks, during which patients are advised to avoid heavy lifting or strenuous activity.
- Laparoscopic Colectomy — Recovery is usually quicker, with hospital stays ranging from 2 to 4 days. Most patients return to normal daily activities within one to two weeks and make a full recovery in about 2 to 4 weeks. This approach generally results in less pain and smaller scars, allowing for a smoother return to daily routines.
What Are the Risks of Colectomy
As with any major surgery, colectomy comes with some risks. While most patients recover without serious issues, it is important to be aware of potential complications:
- Bleeding and Blood Clots — Internal bleeding can occur during or after surgery, and blood clots pose a risk, potentially forming in the legs or travelling to the lungs.
- Infection — Infections can occur at the incision site or internally within the abdomen.
- Organ Damage — In rare cases, nearby structures such as the bladder, small intestine, or ureters may be affected during surgery.
- Scar Tissue and Hernias — Some patients may develop internal scar tissue (adhesions), which can occasionally lead to bowel obstruction. Hernias may also form at the incision site over time.
- Long-term Complications — Some patients may experience changes in bowel habits, urinary function, or sexual function, especially if a stoma is needed.
FAQs






Our Colorectal Surgeons

Dr Dennis Koh
Medical Director & Senior Consultant Surgeon
B Med Sci (Nottingham), MBBS (Nottingham)
MMed (Surgery), FRCS (Edinburgh), FAMS
Dr Dennis Koh is a MOH-accredited and experienced colorectal surgeon with specialised expertise in the management and treatment of colorectal cancer; and currently the Medical Director at Colorectal Practice.
Dr Koh strives to provide a customized treatment plan for each patient, which allows for better outcomes. He also honed his skills in proctology abRd in Geneva, bringing a more diverse touch to his practice.

Dr Sharon Koh Zhiling
Senior Consultant Surgeon
MBBS (Singapore), MMed (Surgery),
FRCS (Edinburgh), FAMS
Dr Sharon Koh is an experienced colorectal surgeon and the former Director of Endoscopy at Alexandra Health. She has subspecialty training in colorectal surgery, minimally invasive surgery, and advanced endoscopy — particularly in the field of colorectal cancer.
Dr Koh completed her fellowship at Cedars-Sinai Medical Centre in the US after being awarded the Academic Medicine Development Award by the National University Hospital.

Dr Pauleon Tan Enjiu
Senior Consultant Surgeon
MBBS (Singapore), MMed (Surgery),
FRCS (Edinburgh), FACS
Dr Pauleon Tan has served in public hospitals for over 15 years and is experienced in minimally invasive surgery and endoscopy. He is also experienced in the treatment for colorectal cancer, and strives to provide the best possible care to his patients.
Dr Tan undertook advanced colorectal surgical training at Japan’s Saitama International Medical Center after being awarded the Ministry of Health – Health Manpower Development Plan (HMDP) Award.